Gastrointestinal Ischemia
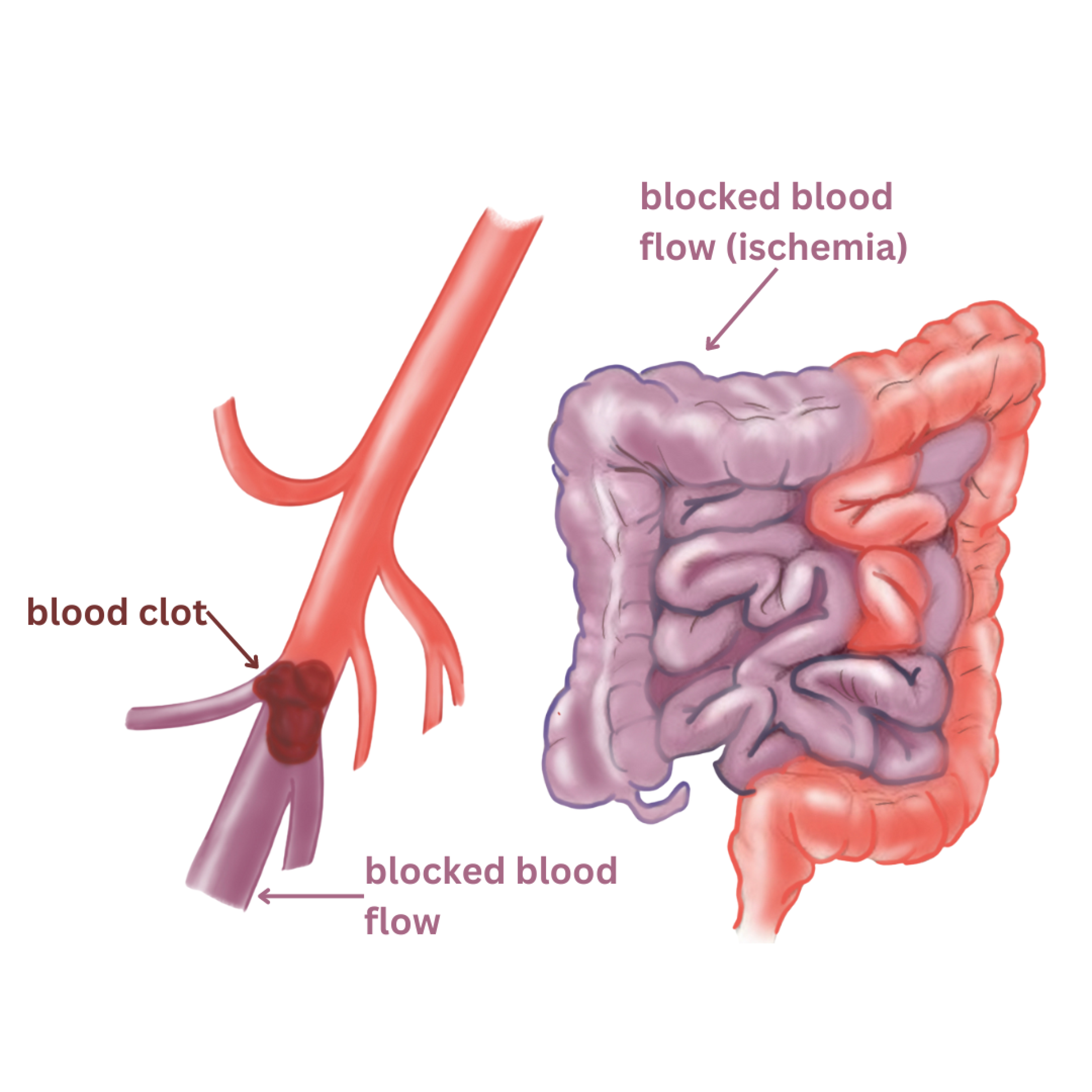
Gastrointestinal Ischemia occurs when the circulation to your gastrointestinal (GI) tract (esophagus, stomach, small intestines, colon, rectum) is compromised or cut off.
These organs are supplied by three major arteries coming off of the aorta–the celiac artery, the superior mesenteric artery, and the inferior mesenteric artery. If these arteries become blocked because of plaque buildup, the organs they supply have decreased blood flow. With decreased blood supply, there is a decrease in oxygen available to your GI organs, leading to cell death and permanent damage–this is called mesenteric ischemia. The most commonly affected organ is the colon.
Risk Factors
Many controllable lifestyle choices and uncontrollable factors such as genetics and aging can put a patient at risk for gastrointestinal ischemia
- Advanced Age (over 50 years old)
- Family History of PAD, Stroke, Heart Disease
- Diabetes
- Smoking (Current smoking or history of smoking)
- High Cholesterol
- High Blood Pressure
- Coagulation disorders
- Obesity
- Personal History of Stroke, Heart Attack
Symptoms
Patients can have two types of gastrointestinal ischemia: acute (sudden) and chronic. Acute mesenteric ischemia and advanced chronic mesenteric ischemia require urgent surgical intervention.
Acute Mesenteric Ischemia is a sudden attack, whereby the organs of your gastrointestinal tract are suddenly deprived of blood and oxygen. Symptoms of such an attack include:
- Sudden and severe abdominal pain
- Bloody stool
- Nausea
- Vomiting
- Fever
Depending on how long it has been since the acute ischemic attack began, there may be frequent bowel movements or no bowel movement, followed by significant fluid loss into the abdomen that results in shock.
Chronic Mesenteric Ischemia
People with chronic mesenteric ischemia have had long term narrowing or blockage of the arteries supplying their gastrointestinal tract. This means their organs have been deprived of blood flow and oxygen transiently for a long period of time. People with chronic GI ischemia may suffer acute intestinal ischemic attacks or experience the following symptoms:
- Abdominal pain or cramps that get worse over time
- Food phobia: 2-3 hours after eating food, patients experience excruciating pain, causing an aversion to eating
- Nausea
- Vomiting
- Malnutrition
- Weight loss
- Bloody diarrhea
Diagnosis
Here at our practice, our doctors and vascular technicians specialize in performing and examining multiple diagnostic tests to assess our patients circulation.
Diagnostic tests include:
Abdominal Ultrasound: This is a noninvasive imaging study performed at our office that uses soundwaves to visualize artery narrowing. This is a very commonly performed test which only takes about 15 minutes to complete.
Computed Tomography Angiogram (CTA): This is a minimally invasive imaging technique completed at an outside facility. This involves IV contrast into your blood vessels and CT scanning to accurately evaluate the extent of your stenosis. Compared to MRAs, CTs are preferred for optimal visualization.
Magnetic Resonance Angiography (MRA): This minimally invasive imaging technique uses magnetic resonance to visualize the blood vessels in your body. It may involve IV contrast into your blood vessels to allow for visualization.
Mesenteric Angiogram: This is a minimally invasive procedure performed at the hospital. The procedure begins with a small puncture made to access the femoral arteries and guided to the artery of interest. Contrast dye is delivered through this tube. Throughout the procedure, the vascular surgeon uses real-time x-ray images and contrast dye injections to visualize the circulation and any blockage in the artery of interest.
Treatment Options
Nonsurgical Treatment:
For patients with mild blockages without notable symptoms, our physicians and team at BEVSA work with you to develop a treatment plan to prevent the progression of your disease.
Risk Factor Modification: Tobacco use damages the arterial walls which makes it easier for plaque to build up and cause complications such as increased abdominal ischemia. If you need help quitting smoking, our physicians will help you obtain information on medication, nicotine replacement products, and programs to make it easier
Diet and Activity: It is important to maintain a diet low in saturated fat, cholesterol, and sodium. Foods with these components can elevate cholesterol levels making it more likely for plaque to build up in the artery and cause narrowing. Our physicians will work with you to develop a customized, feasible, exercise plan and dieting.
Medication Management: Risk factors include elevated cholesterol/fat levels and type 2 diabetes. Statins have been shown to manage cholesterol/fat levels, stabilize plaque, and reduce the risk of plaque buildup. In addition patients with type 2 diabetes should engage in good glycemic control and work with their physician to achieve low levels of A1C. Our physicians will work with you to ensure you are on the proper medication regimen to lessen your risk of ischemic changes to the abdominal vessels.
Surgical Treatment
Minimally Invasive Procedure: This is an angiogram procedure performed at the hospital that only involves a small incision in the groin. A catheter (long, flexible tube) is then inserted in the arm to inject contrast dye into the arteries of the abdomen. The dye and real time x-ray images are used to identify where blockages in the leg arteries are occurring. After the blockage is identified, the vascular surgeon may use angioplasty or stenting to improve the circulation. Angioplasty is when a small balloon is inflated inside of the vessel to widen it. A stent, which is a hollow, metal scaffold, is sometimes placed permanently inside the artery to hold it open. There are also drug eluting stents which release drugs that fight any further plaque buildup in the stent itself.
Surgical Bypass: This is an open surgical procedure performed at the hospital for patients that have full blockage of the artery that cannot be treated, or have failed to be treated, with a minimally invasive procedure. A bypass graft is placed to re-route the blood around the blocked portion of the artery and creates better circulation for the reduced portion of the vessel. This is a longer procedure that requires general anesthesia and medical clearance.