May-Thurner Syndrome
May-Thurner Syndrome increases your risk for blood clots in your lower extremities.
https://www.gethealthyveins.com/2021/01/13/may-thurner-syndrome-an-unknown-vascular-condition/
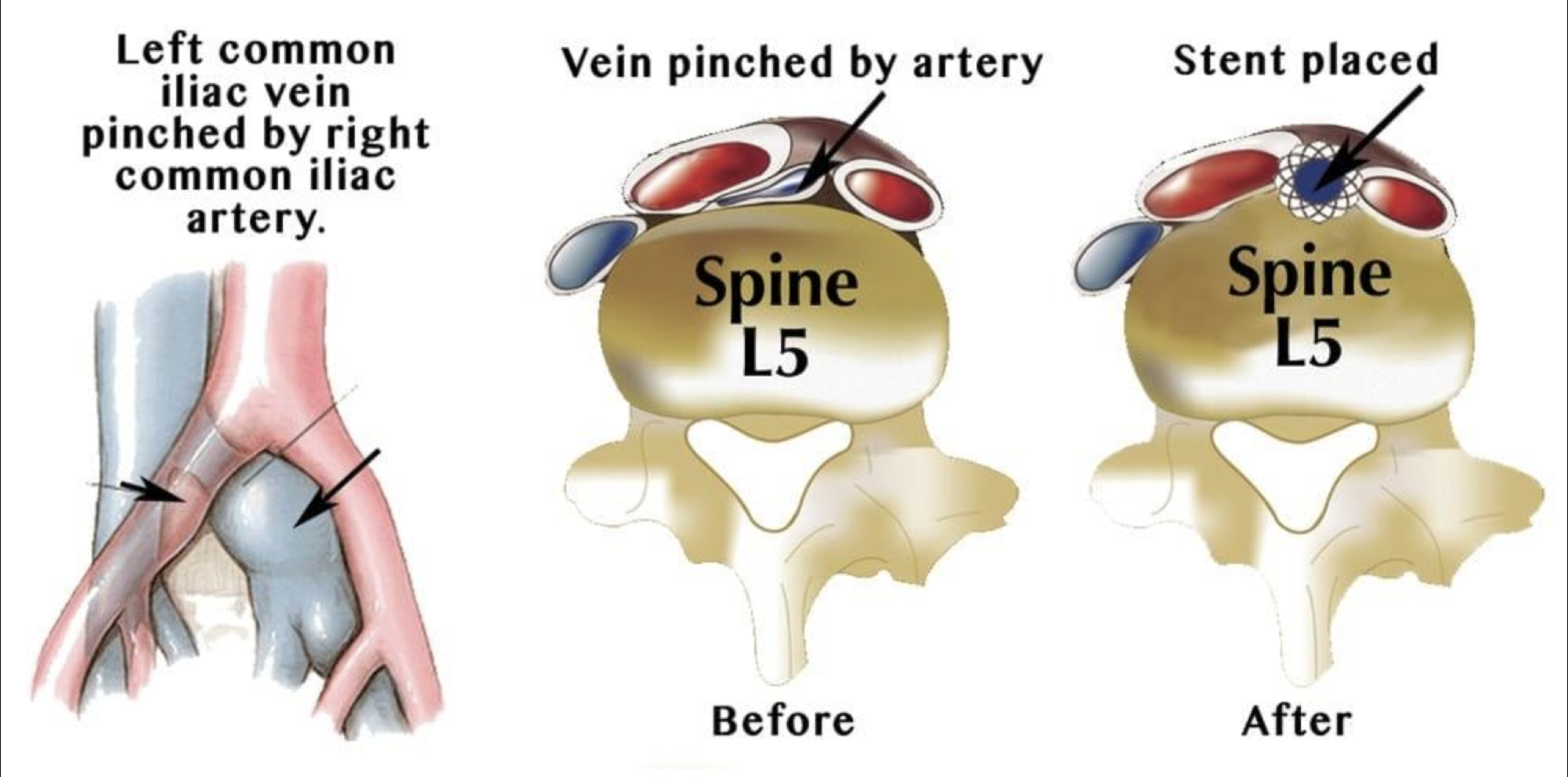
May-Thurner Syndrome, also known as Iliac Vein Compression Syndrome, is a condition in which a person's iliac artery compresses their iliac vein, limiting blood flow from the lower extremity back to the heart. This limited blood flow can lead to vessel narrowing, scarring, and the development of blood clots in the veins of the leg, a condition known as Deep Vein Thrombosis (DVT), which can cause pain and swelling, and increases risk of pulmonary embolism. Most often, the left common iliac vein is compressed by the right common iliac artery, but May-Thurner Syndrome can occur with either the left or right iliac veins and affect either leg.
Symptoms
Most people don't know that they have May-Thurner Syndrome until they develop Deep Vein Thrombosis (DVT).
Symptoms of DVT caused by May-Thurner Syndrome include:
- Leg swelling
- Pain or tenderness in one's leg
- Redness and discolouration
- Enlargement of veins on leg
Diagnosis
If you present with symptoms of DVT, your physician may suspect May-Thurner Syndrome.
If you experience leg swelling, pain, discolouration, and other symptoms of DVT, your physician may suspect May-Thurner Syndrome and will order diagnostic imaging, likely a CT, to look at the anatomy of your vasculature and see if your iliac artery is compressing your iliac vein.
Non-Surgical Treatment
There are several non-surgical interventions that can help manage DVT caused by May-Thurner Syndrome.
Anticoagulation
If you are diagnosed with May-Thurner Syndrome, you are at risk of developing a blood clot (DVT) in your legs. Anticoagulants are used as a protective measure to prevent further DVTs from forming and causing worsening of symptoms. In fact, the risk of extension of a patient's blood clot is significantly increased if anticoagulants are not used within the first 24 hours of symptoms. The duration of blood thinner use is usually a minimum of 3 months after being diagnosed with a DVT and can extend longer depending on the patient's risk of developing additional DVTs. Blood thinners protect a patient from clot formation and allow the body to dissolve the clot that is present in the veins. Our surgeons will work with you to determine the appropriate blood thinner type, dosage, and duration of use to keep you protected from DVT.
Compression Stockings
For patients with significant swelling in their legs due to DVT, they may be prescribed compression stockings. Compression stockings are fitted socks that help squeeze blood up your legs and alleviate swelling from a vein being blocked with a DVT. If the swelling is in the calf, knee high socks may be appropriate. If the swelling is in the thigh there are thigh high stockings as well. Our vascular surgeons will work with you to give you a prescription for compression stockings. Prescription grade compression stockings are custom fitted, and apply more pressure than regular over the counter compression stockings.
Leg Elevation and Exercise
For patients with significant swelling in their legs due to DVT, leg elevation can be an effective lifestyle change to help alleviate swelling. It is important that patients with a DVT avoid sitting or laying for extended periods of time as this allows blood to pool around the calves and ankles and can worsen swelling. Patients should aim to elevate their affected leg above the level of their heart any time they are sitting or laying down. In addition, leg exercises can help activate the calf pump which squeezes blood in the veins towards the heart and can lessen swelling. Aerobic activity such as walking, stationary biking is encouraged. If you are stuck sitting for a long period it is important to stand up and walk around periodically to activate the calf pump.
Surgical Treatment
Your physician may determine that it is best to intervene with a minimally invasive surgical procedure to alleviate the compression of your iliac vein or to remove a clot from your leg veins that has occurred as a result of your May-Thurner Syndrome.
Surgical Treatments for Vein Compression
Angioplasty and Stenting: Angioplasty is a procedure in which a balloon is used to open a narrowed vein. In patients with May-Thurner Syndrome, angioplasty may be used to open up the compressed iliac vein. Following angioplasty, a stent is often placed to keep the compressed vein open.
During the procedure, a balloon-tipped catheter, a long, thin plastic tube, is guided into the veins to access the compressed vessel. The balloon is then inflated to open the vessel, deflated, and removed. With vascular stenting, a stent is placed in the newly opened vein to help it remain open. The stent acts as a scaffold to keep the walls of the vein from collapsing.
This procedure can be done at our AccessCare outpatient facility with discharge home the same day.
Surgical Treatments for DVT
In addition to blood thinners, leg elevation, and exercise, surgical treatment may be necessary to remove the blood clot or prevent it from traveling to the lungs. Fortunately, you have many minimally invasive, convenient treatment options available at BEVSA that our surgeons are well trained and experienced in. Eligible patients usually have a DVT that is above the knee in the thigh or groin area and have been diagnosed with a DVT in the past month.
Thrombolysis: Thrombolysis is a procedure in which a small puncture is made in the back of the knee to access the vein. A catheter (long, thin tube) is then guided through the puncture to the site of the clot. “Clot busting” medication is then delivered to the DVT in the vein to dissolve the blood clot and re-open the vein. Sometimes, a small device is inserted in the vein to mechanically break up the clot and/or a stent is placed in the vein to keep it open and prevent swelling. This procedure occurs at Buffalo General Hospital and usually requires a patient to stay overnight to allow the clot busting medication to fully dissolve the clot.
Thrombectomy: Thrombectomy is a procedure in which a small puncture is made in the back of the knee to access the vein. A catheter (long, thin tube) is then guided through the puncture to the site of the clot. A small device is then guided on the catheter to the site of the clot. The device is then controlled by the vascular surgeon to mechanically break up, collect, and remove the clot. This procedure can be performed on its own or after a thrombolysis in the hospital. In addition, thrombectomy can be performed safely and effectively at our outpatient facility, Access Care, with discharge home the same day.
Inferior Vena Cava (IVC) Filter: The inferior vena cava (IVC) is the major vein that transports deoxygenated blood from the legs to the heart and lungs. Blood clots that occur in the veins in the legs can potentially break off and travel through the IVC to the lungs and cause a life threatening condition called a pulmonary embolism. An IVC filter is a small, wired device that is placed in the IVC to filter blood. The IVC filter allows blood to travel through it while collecting blood clots and preventing them from traveling to the lungs. The filter can be placed temporarily or permanently depending on the patient's risk factors for subsequent DVTs. The IVC filter is placed through a small incision in a vein in the neck or groin and guided to the IVC. The filter has a hook on the top of it for retrieval if necessary. The procedure can be performed safely and effectively at our outpatient facility, Access Care, with discharge home the same day.
Treatment Options for May-Thurner Syndrome
Thrombectomy and Venous Stenting
- Minimally Invasive Venogram
- Vein Clot (DVT) Removal
- Swelling Alleviation