Deep Vein Thrombosis (DVT)
Whether Young, Old, Sick or Healthy, Almost Anyone can be Affected by a DVT
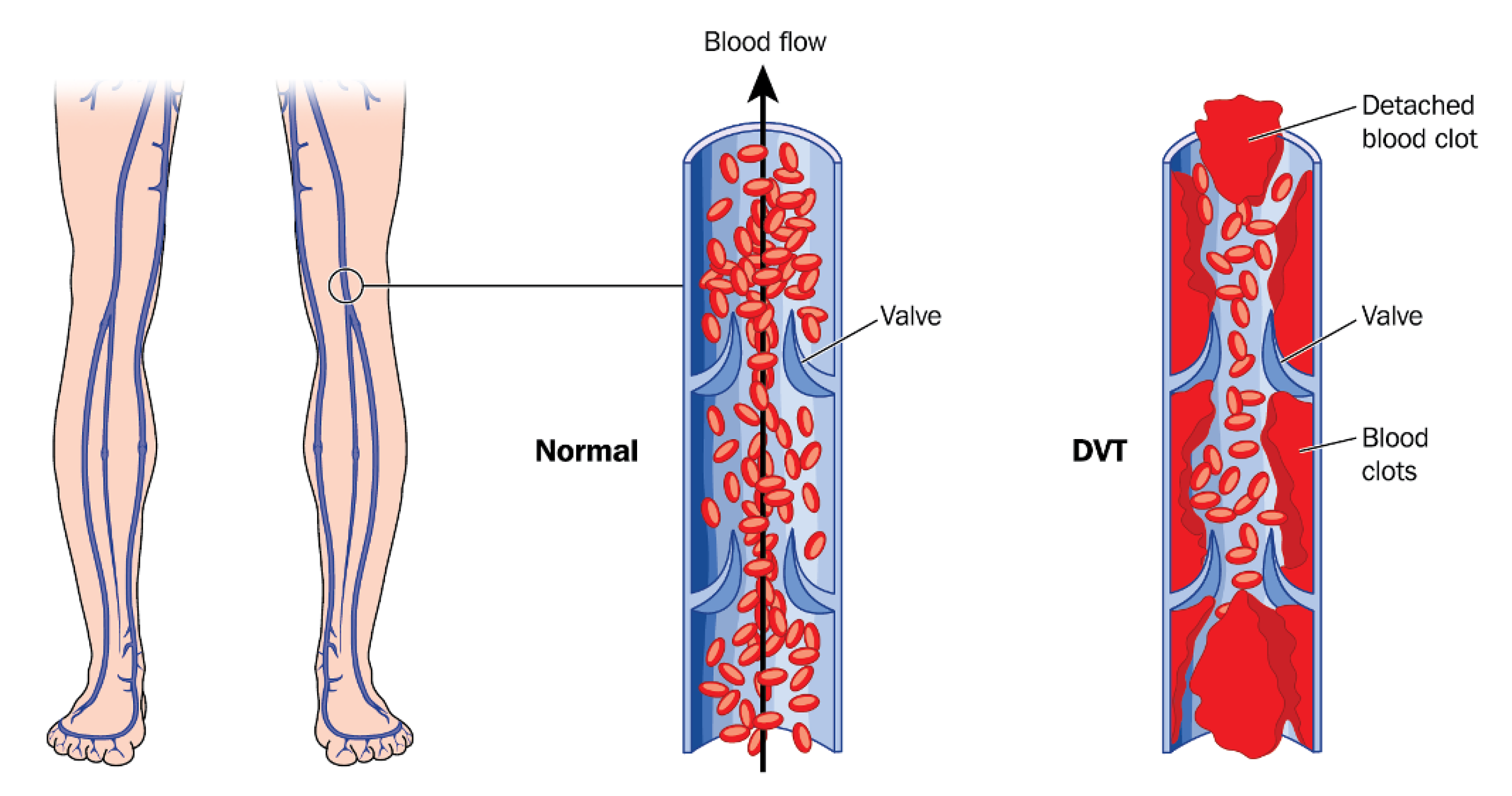
The veins are blood vessels that contain valves and are responsible for transporting deoxygenated blood from the periphery to the heart and lungs. A deep vein thrombosis (DVT) is a blood clot that occurs in the veins usually as a result of blood pooling together around a valve in the vein. The clot can either partially or fully block the vein from transporting blood which results in swelling in the tissue below the clot. DVTs usually occur in the lower leg, thigh or pelvis, however they can also occur in other parts of the body including the arms.
A DVT in the leg usually causes swelling, tiredness, and discomfort, however it can also pose a life threatening condition called pulmonary embolism. A pulmonary embolism occurs when a portion of the blood clot in the leg breaks off and travels to the lungs. The clot then becomes lodged in the lungs and can restrict a patient's ability to breathe. Unfortunately, sudden death is the first symptom in about 25% of people who have a pulmonary embolism.
Having a DVT can also lead to long term complications called post thrombotic syndrome (PTS). PTS occurs when the clot damages the valves in the veins, resulting in long term swelling, discoloration, ulcers and pain. Approximately one third of people with a DVT will develop PTS. This number is increased for patients who do not undergo any treatment. In addition, having a DVT puts a person at risk of developing another DVT in the future. About one third of people who have a DVT/PE will have a recurrence within 10 years.
Risk Factors
The main components that put a person at risk of developing a DVT are prolonged immobility and/or an injury to the veins. Alarmingly, this set of criteria encompasses a vast majority of our population and puts many people at risk for DVT, regardless of their age or health. People who are seated for a long time during a trip or lie flat during or after a surgery are at risk for DVT because these situations promote blood to pool in the veins and potentially form a clot. In addition, uncontrollable factors such as cancer and genetics can put a person at risk for clotting.
- Extended period of not moving (long trip, surgery)
- Overweight/Obesity
- Genetic Condition (Blood Clotting Disorder)
- Cancer
- Pregnancy
- Birth Control Pills
- COVID-19
Symptoms
From minor discomfort to life threatening symptoms such as shortness of breath, patients with DVTs experience a wide variety of symptoms. A DVT usually forms in one of the legs and symptoms of DVT are restricted to the affected leg. Regardless of the severity, It is important to call your doctor right away if you are experiencing symptoms of DVT. If you are experiencing symptoms of pulmonary embolism go to the emergency room right away.
Symptoms of DVT
- Leg swelling
- Aching or Heaviness in leg
- Redness or discoloration of skin
- Tightness of skin
Symptoms of Pulmonary Embolism
- Shortness of breath
- Chest Pain
- Cough
- Fast Heartbeat
- Feeling Dizzy or Fainting
Diagnosis
When a patient reports leg swelling, discomfort, or redness to their physician, they are often sent to obtain noninvasive vascular studies to determine if a clot is present in the veins. Here at AccessCare, our doctors and vascular technicians specialize in performing and examining diagnostic tests to assess our patients' DVTS.
Venous Ultrasound: This is a noninvasive, imaging study performed at our office that uses sound waves to visualize vessel contents in the leg veins for signs of clot. This is one of the most common DVT tests performed at our office and takes about 10 minutes.
CT Venogram Scan: This is an imaging study that combines x-ray technology and contrast use. The dye is injected through a small IV line started in your arm and the test does not require any sedation. This test is usually performed for patients who have extensive clot to determine the location of the clot and if they are a candidate for surgery.
Non Surgical DVT Treatment Options
Depending on the location and severity of a patient’s DVT, it may be decided that the best course of treatment is nonsurgical therapy consisting of a combination of medication, compression stockings, and leg elevation.
Blood Thinners: After a venous ultrasound confirms that a patient is suffering from a blood clot (DVT), they are usually prescribed blood thinner medication (anticoagulant). Anticoagulants are used as a protective measure to prevent further DVTs from forming and causing worsening of symptoms. In fact, the risk of extension of a patient's blood clot is significantly increased if anticoagulants are not used within the first 24 hours of symptoms. The duration of blood thinner use is usually a minimum of 3 months after being diagnosed with a DVT and can extend longer depending on the patient's risk of developing additional DVTs. Blood thinners protect a patient from clot formation and allow the body to dissolve the clot that is present in the veins. Our surgeons will work with you to determine the appropriate blood thinner type, dosage, and duration of use to keep you protected from DVT.
Compression Stockings: For patients with significant swelling in their legs due to DVT, they may be prescribed compression stockings. Compression stockings are fitted socks that help squeeze blood up your legs and alleviate swelling from a vein being blocked with a DVT. If the swelling is in the calf, knee high socks may be appropriate. If the swelling is in the thigh there are thigh high stockings as well. Our vascular surgeons will work with you to give you a prescription for compression stockings. Prescription grade compression stockings are custom fitted, and apply more pressure than regular over the counter compression stockings.
Leg Elevation and Exercise: For patients with significant swelling in their legs due to DVT, leg elevation can be an effective lifestyle change to help alleviate swelling. It is important that patients with a DVT avoid sitting or laying for extended periods of time as this allows blood to pool around the calves and ankles and can worsen swelling. Patients should aim to elevate their affected leg above the level of their heart any time they are sitting or laying down. In addition, leg exercises can help activate the calf pump which squeezes blood in the veins towards the heart and can lessen swelling. Aerobic activity such as walking, stationary biking is encouraged. If you are stuck sitting for a long period it is important to stand up and walk around periodically to activate the calf pump.
Surgical DVT Treatment Options
In addition to blood thinners , leg elevation, and exercise, surgical treatment may be necessary to remove the blood clot or prevent it from traveling to the lungs. Fortunately, you have many minimally invasive, convenient treatment options available at AccessCare that our surgeons are well trained and experienced in. Eligible patients usually have a DVT that is above the knee in the thigh or groin area and have been diagnosed with a DVT in the past month. These procedures are performed safely and effectively at AccessCare with discharge home the same day.
Thrombectomy: Thrombectomy is a procedure in which a small puncture is made in the back of the knee to access the vein. A catheter (long, thin tube) is then guided through the puncture to the site of the clot. A small device is then guided on the catheter to the site of the clot. The device is then controlled by the vascular surgeon to mechanically break up, collect, and remove the clot.
Venous Stenting: In addition to a blood clot, sometimes patients with a DVT have an underlying compression of their vein. A compressed vein limits blood flow out of the leg, and can cause increased swelling even after the blood clot is removed. Therefore a stenting procedure is performed where a small puncture is made in the back of the knee to access the compressed vein. A catheter (long, thin tube) is then guided through the puncture to the narrowed vein. A stent is then guided along the catheter and placed inside the vein. The stent can help alleviate swelling and prevent blood from pooling in the veins and causing an additional DVT.
Inferior Vena Cava (IVC) Filter: The inferior vena cava (IVC) is the major vein that transports deoxygenated blood from the legs to the heart and lungs. Blood clots that occur in the veins in the legs can potentially break off and travel through the IVC to the lungs and cause a life threatening condition called a pulmonary embolism. An IVC filter is a small, wired device that is placed in the IVC to filter blood. The IVC filter allows blood to travel through it while collecting blood clots and preventing them from traveling to the lungs. The filter can be placed temporarily or permanently depending on the patient's risk factors for subsequent DVTs. The IVC filter is placed through a small incision in a vein in the neck or groin and guided to the IVC. The filter has a hook on the top of it for retrieval if necessary.
Angiojet Thrombectomy Procedure
This is an example of a minimally invasive treatment procedure for patients with DVT. The thrombectomy procedure uses a device that travels over the clot in the vein and aspirates, or sucks, clot out of the vein to open up the vein and reduce leg swelling.
Frequently Asked Questions
What determines if I am eligible for a surgery for my DVT?
If your DVT is located below the knee, it is usually treated nonsurgically with blood thinners and leg elevation. This is because the risk of the clot traveling to the lungs is low and the veins are too small to guide wires and devices through them. Above the knee DVT can be surgically treated because this condition poses an increased risk of pulmonary embolism and subsequent leg pain and swelling. In addition, the veins above the knee are large enough for surgery. Furthermore, the above the knee DVT has to have occurred within a few weeks of surgery. This is because the new clot is fresh and squishy and can be removed easily. The longer the clot is in the vein, the harder it becomes and more difficult it is to remove.
What are the side effects of being on blood thinners?
Most patients do not report any side effects while being on a blood thinner. However, some of the most common side effects that may occur are easy bleeding/bruising, stomach discomfort/pain, and diarrhea. To lower the chance of getting cut, bruised, or injured, use caution with sharp objects like razors and nail cutters, and avoid activities such as contact sports. If you are having any issues with your medications, be sure to contact your prescribing physician.
Do IVC filters protect against DVT?
IVC filters do not protect against a DVT. IVC filters prevent a DVT in the leg from traveling to the lungs and causing a potentially life threatening condition called pulmonary embolism. You may still experience swelling, discomfort, discoloration in your legs even with an IVC filter placed.
Treatment Options for Deep Vein Thrombosis (DVT)
Thrombectomy and Venous Stenting
- Minimally Invasive Venogram
- Vein Clot (DVT) Removal
- Swelling Alleviation
