Angiogram
Minimally Invasive Treatment Options for Your Legs
 We are excited to offer you numerous minimally invasive treatment options to improve circulation in your legs to alleviate pain and heal wounds. Our surgeons are always keeping up with the latest plaque removal technology options, and we will listen to your story and analyze test results to assess which option works best for your needs. These treatment options have been safely and effectively performed at our outpatient procedure lab, AccessCare Vascular for over a decade.
We are excited to offer you numerous minimally invasive treatment options to improve circulation in your legs to alleviate pain and heal wounds. Our surgeons are always keeping up with the latest plaque removal technology options, and we will listen to your story and analyze test results to assess which option works best for your needs. These treatment options have been safely and effectively performed at our outpatient procedure lab, AccessCare Vascular for over a decade.
Who is Eligible For a Minimally Invasive Procedure?
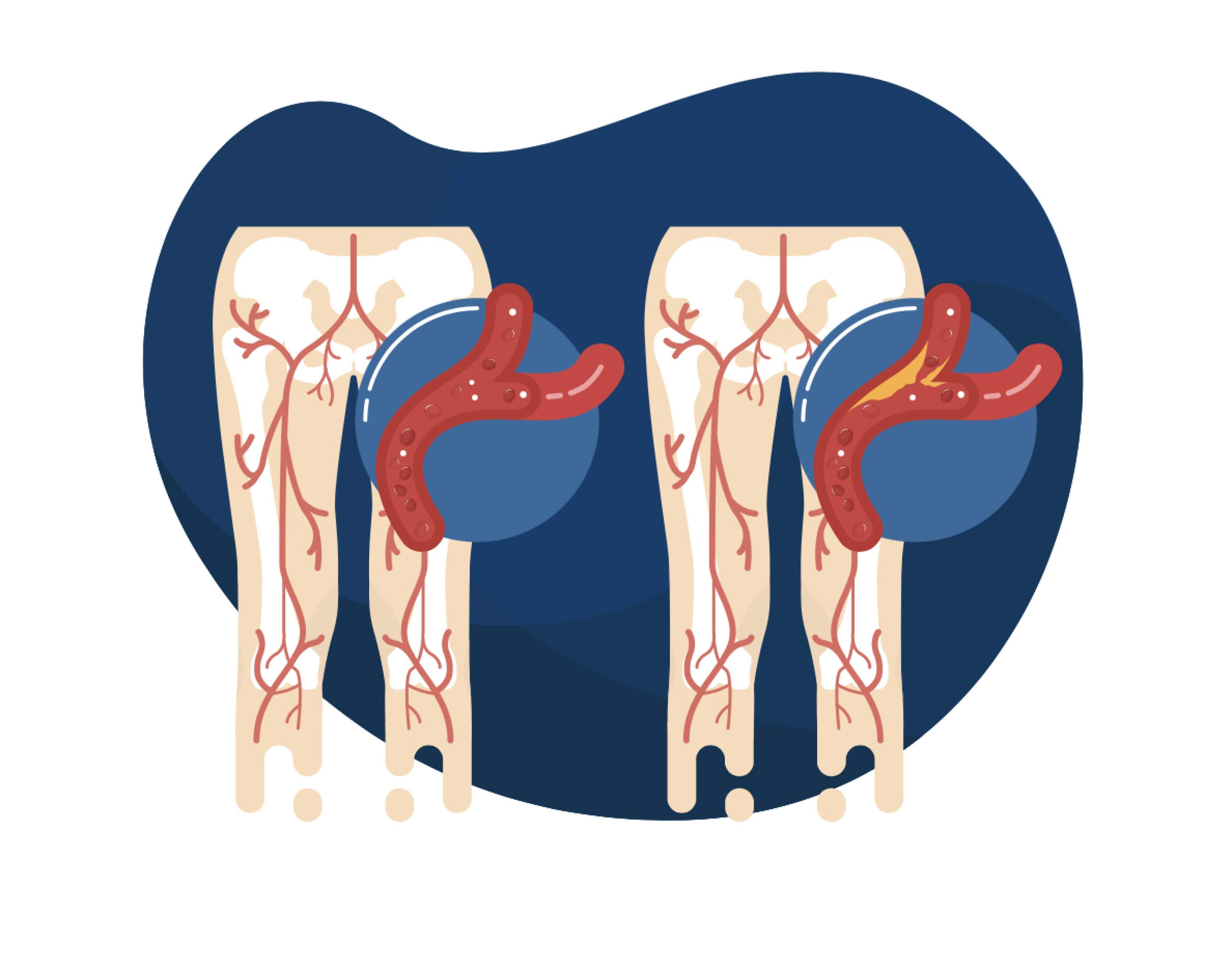
Peripheral Arterial Disease (PAD) is a disease of the arteries which occurs when plaque begins to buildup in the artery wall and limit blood flow, usually in the legs. When plaque builds up in the leg arteries, patients do not receive enough blood and oxygen to their leg muscles and feet which can result in symptoms such as leg pain while walking, non healing wounds, and discoloration of the feet.
Often, patients with these symptoms come to our office and first undergo non-invasive diagnostic studies to determine how much plaque is in the arteries and the amount of blood that is reaching the patients legs and feet. Depending on the studies and your symptoms, your vascular surgeon will determine if your arterial disease is severe enough for intervention.
For some patients with mild arterial disease, non surgical recommendations such as medication, exercise, smoking cessation, diet may be discussed. For patients with more severe arterial disease and symptoms, a minimally invasive procedure may be necessary to widen the blood vessel and clean out any plaque to improve blood flow in the legs. For qualifying patients, a minimally invasive procedure at AccessCare is explored before major surgery at the hospital. However, sometimes imaging studies will indicate that the patient has too much plaque in their arteries for a minimally invasive procedure, and a more extensive procedure would be necessary such as an endarterectomy, or surgical bypass in the hospital.
Minimally Invasive Treatment Options
Angiogram: An angiogram is one of the best tools utilized by vascular surgeons to visualize blood flow in the arteries. An angiogram begins with a small, minimally invasive incision in the groin to access the leg artery. Next, a small needle is used to make a puncture in the femoral artery. A catheter (long, thin, flexible tube) is carefully guided into the artery and positioned at the area where plaque may be present. The surgeon then injects contrast dye through the catheter which is then visualized by x-ray machinery. This allows the surgeon to visualize the inside of the artery and determine the location and extent of arterial blockages and which kind of treatment is necessary. This is the first step of any minimally invasive treatment.
Angioplasty: When an arterial blockage is discovered, your surgeon may use balloon angioplasty to help widen the vessel. A wire is first guided across the area of plaque, and a small, deflated balloon is then placed in the area of narrowing in the artery. The surgeon then inflates the balloon to push the plaque up against the artery wall to widen the blood vessel. When the balloon is deflated, the blood vessel is now wider and able to allow more blood to pass through it. Contrast dye is then injected through the artery to confirm the results.
Stenting: Sometimes, an angioplasty is not sufficient to keep an artery open and a more permanent solution is necessary. A stent acts as a hollow, metal, scaffold by "propping open" an artery. A stent is guided to the area of the plaque in the artery with a catheter and is then deployed to push the plaque against the wall and increase the diameter of the artery. Stents are very flexible and are designed to twist and turn with body and artery movement.
Atherectomy: Instead of pushing plaque against the wall, the atherectomy procedure is used to mechanically remove plaque from the artery. First, A small, rotating burr is guided to the area of plaque with a catheter. The vascular surgeon then activates the burr which begins to rotate and break apart the plaque. The surgeon may need to do multiple passes of the plaque to "shave" the plaque off of the vessel wall. The burr is specially designed to only engage with plaque in the artery and it avoids damaging the vessel wall. Depending on the device used, the plaque particles are either sucked out of the artery or they are ground up into microscopic pieces and eliminated by the body's natural mechanisms.
Atherectomy Procedure
The Atherectomy procedure uses a small, rotating burr to push plaque up against the blood vessel wall and widen the artery to increase blood flow. This procedure is done minimally invasively with a small incision in the groin.
Angiogram Procedure
Jamie H., our head nurse at AccessCare, explains what an angiogram is and what patients at AccessCare can expect before, during, and after their procedure at our facility.
Procedure Details
Before The Procedure: Plan on arriving to our Access Care Facility 1-2 hours before the procedure. Patients cannot drive to the facility and they have to be dropped off by someone else. Before the procedure, patients are prepped in our recovery room. A nurse will administer medication to you that will act as a sedative. This is called conscious sedation, which is used to relax the patient and causes many patients to fall asleep during the procedure. In addition, local anesthesia or numbing medication is applied to the skin on the groin where the surgeon will make a minimally invasive incision.
During The Procedure: Patients are then transferred from our recovery area to the procedure room. Our procedure room has its own dedicated staff of nurses, x-ray technicians, and support staff to assist the surgeon throughout the procedure. Depending on the amount of arterial disease, the procedure can last anywhere between 1-2 hours. During the procedure, you must lie flat on their back. The surgeon will utilize angiogram, and a combination of angioplasty, stenting, and atherectomy to treat your peripheral arterial disease. At the end of the procedure, a closure device is used to close the artery and prevent any bleeding outside of the artery. Sometimes manual pressure is held over the groin to stop bleeding instead of a closure device.
After The Procedure: Patients are then transferred from the procedure room back to the recovery room. You must lie flat for another 2-3 hours after the procedure to ensure that the artery closes properly. Afterwards, you are discharged from our facility the same day as your procedure and you must have another person pick you up from the facility. Most patients report being back to normal activity within a few days after the procedure.
Patient Stories
Here at AccessCare, we pride ourselves on engaging with our patient’s stories and feedback. The following stories help highlight how our superior vascular care and compassion translates from our office to improving the everyday lives of our patients. We hope these stories provide comfort to our patients and their families and illustrate how our team at AccessCare goes above and beyond for our patients everyday.
Betty had leg pain while walking: Fortunately, she discovered AccessCare Vascular-Click the Link to learn more!
Frequently Asked Questions
Will I be able to resume normal activities after my procedure?
All of our patients arrive and leave the same day. Depending on the type of procedure, there may be some minor, short term restrictions. This mostly includes driving, heavy lifting and/or strenuous activities. We will explain all of this information in detail plus provide written instructions the day of your procedure.
Does my driver need to stay during the procedure?
No. We can contact your driver with the approximate time of your discharge.
Will I be put to sleep for this procedure?
No. We do not use general anesthesia. We use conscious sedation or “twilight”. This sedations ensures that you will feel comfortable throughout your procedure. It often relaxes patients to the point where they fall asleep on their own.
Will the procedure hurt?
Our mission for the last decade has been to make outpatient minimally invasive procedures, a safe and painless experience. All of our procedure are done through a small puncture in the groin to access the artery. Numbing medication is applied to the area before the procedure to help prevent any associated pain.

AccessCare Procedure Room
AccessCare Procedure Room

AccessCare Recovery Area
AccessCare Recovery Area
Conditions Treatable with Angiogram
Peripheral Arterial Disease (PAD)
- Leg Pain While Walking
- Non-Healing Wounds
- Plaque in the Arteries